Carotid Artery Disease
An often silent cause for nearly 1/3 of all strokes.
Disease Overview
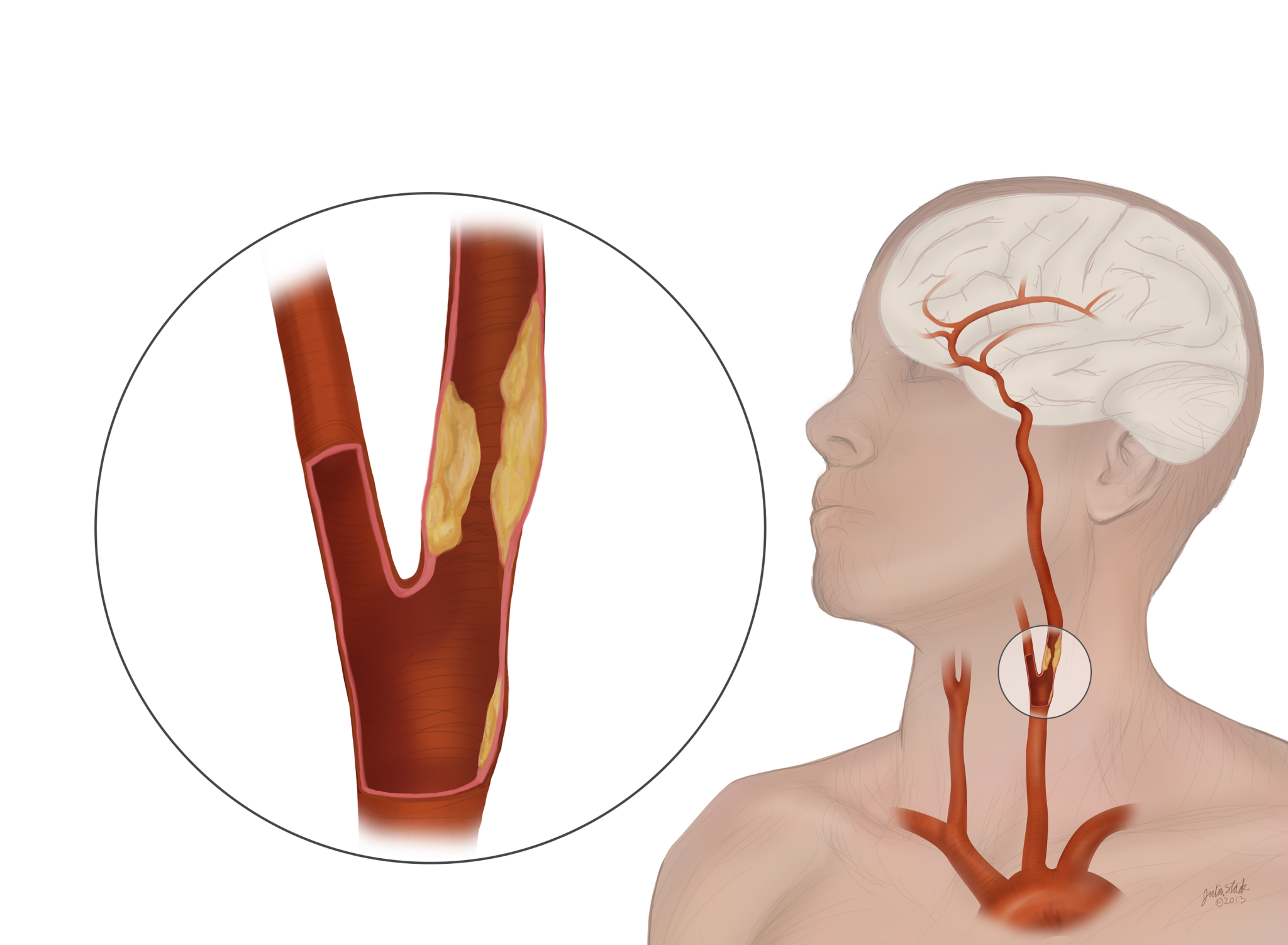
The carotid arteries are vital blood vessels in your neck that deliver oxygen-rich blood to your brain. Carotid artery disease occurs when the carotid arteries become clogged with fatty material called plaque. When plaque builds up in the carotid arteries, they begin to narrow and slow down blood flow, potentially causing a stroke if blood flow stops or plaque fragments travel to the brain.
Risk Factors
Carotid artery disease is often silent and does not always present with symptoms. Physicians can screen patients based on risk factors like high blood pressure, diabetes, obesity and smoking. Sometimes, patients are screened for carotid artery disease if the doctor knows the patient has vascular disease elsewhere in the body. Blockages can also be found when a physician hears a sound through a stethoscope placed on the neck. The sound is caused by blood flowing past the blockage:
You may be at risk if you have two or more of the following:
High cholesterol
Large amounts of cholesterol in the blood can build up and cause blood clots — leading to a stroke.
High blood pressure
This is the leading cause of stroke. Know your blood pressure and have it checked every year.
Tobacco smoking
The nicotine and carbon monoxide in cigarette smoke damage the cardiovascular system and pave the way for a stroke.
Family history
If your close blood relations have had a stroke, you are at higher risk of stroke.
Symptoms
Called the silent killer, often the first symptom for a patient at risk for stroke is a stroke itself or a “mini-stroke” called a transient ischemic attack (TIA). A TIA is a temporary stroke that resolves itself in 24 hours or less. It is considered a warning sign for a full-blown stroke.
To prevent a stroke, talk to your physician about your risk factors. Physicians can screen patients based on risk factors like high blood pressure, diabetes, obesity and smoking. Sometimes, patients are screened for carotid artery disease if the doctor knows the patient has vascular disease elsewhere in the body. Blockages can also be found when a physician hears a sound through a stethoscope placed on the neck. The sound is caused by blood flowing past the blockage.
If someone is having stroke-like symptoms (weakness/numbness on one side, loss of eyesight/speech, garbled speech, dizziness or fainting), they should seek immediate medical attention and be evaluated for carotid artery disease. If you suspect a stroke, remember to act F.A.S.T.
Face drooping
Look for an uneven smile.
Arm weakness
Check if one arm is weak.
Slurred speech
Listen for slurred speech.
Time to call 9-1-1
Right away.
Treatment Options
There are four basic treatment options for patients with carotid artery stenosis. It is important to inform your doctor about your entire medical history. Be sure to ask your doctor to explain the risks and benefits of your treatment options and answer any questions you or your family may have.

Medical Therapy
Managing your carotid artery disease with medication.
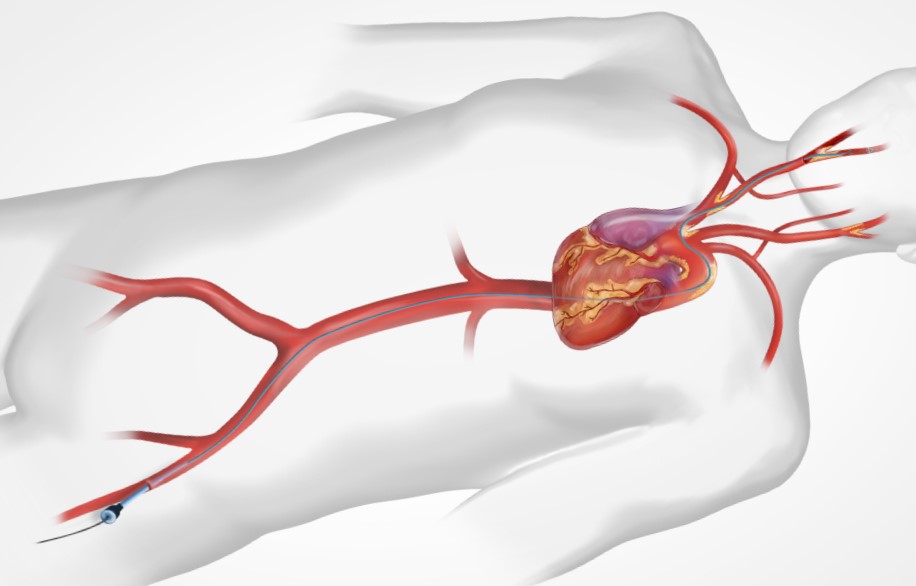
Transfermoral Carotid Artery Stenting

Carotid Endarterectomy
Surgical treatment option to reduce the risk of stroke.
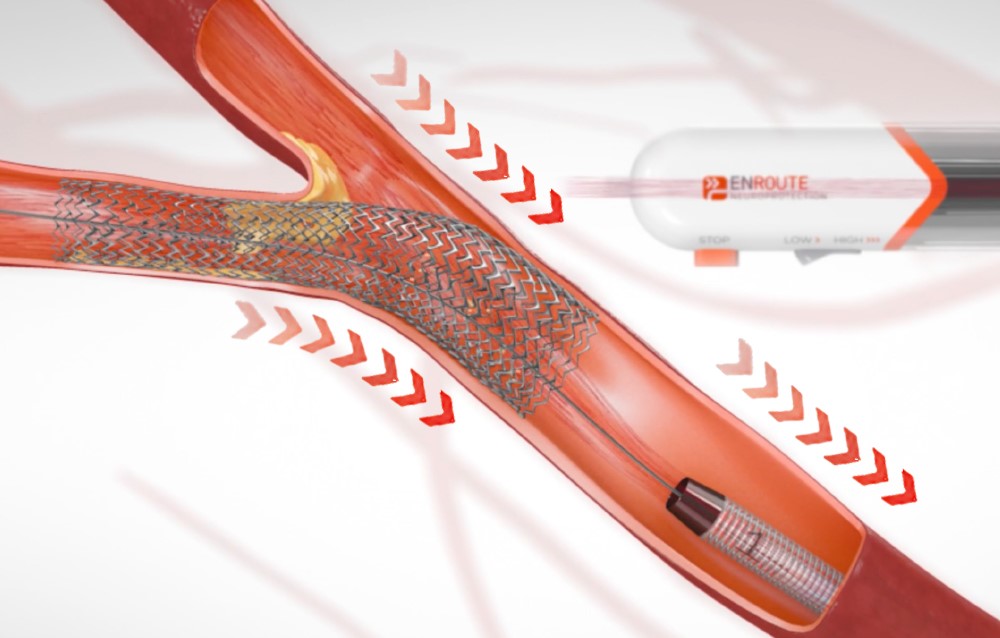
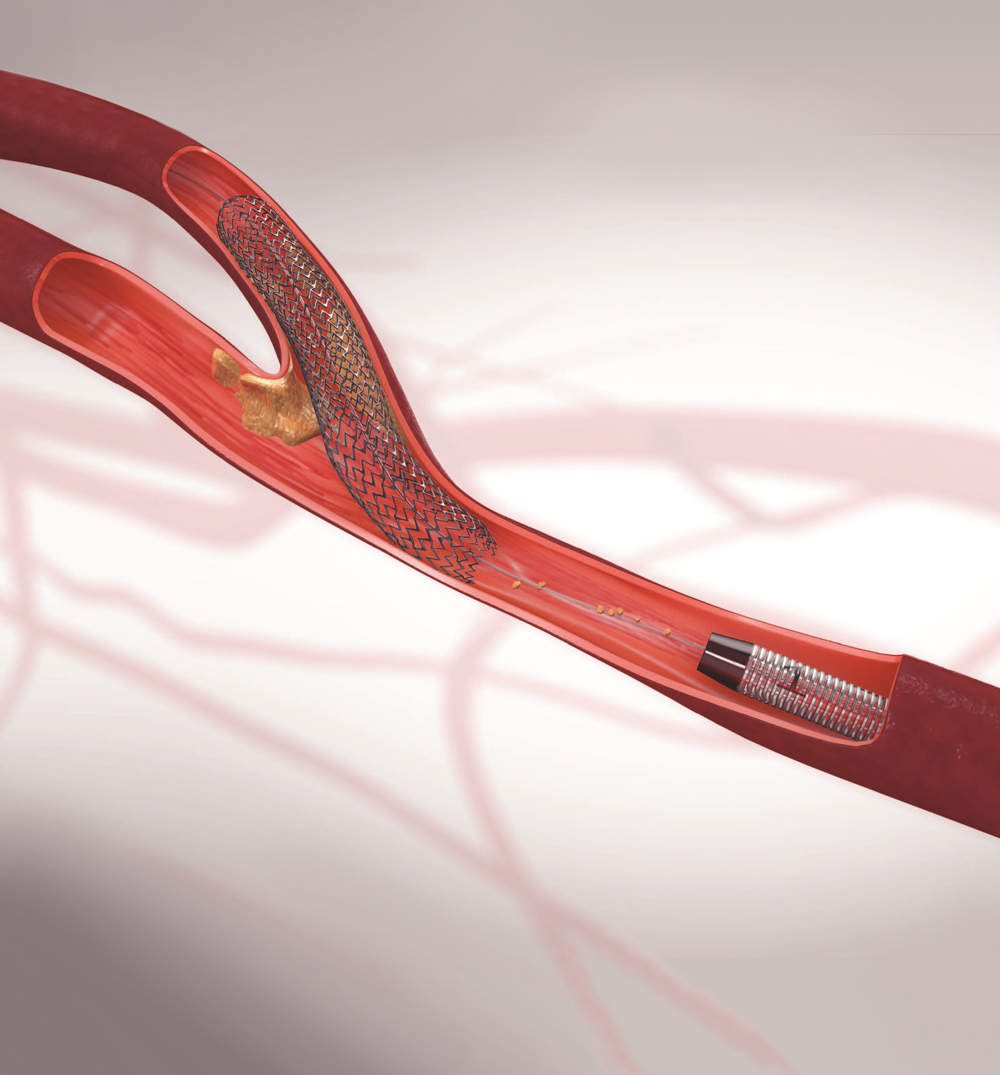
TransCarotid Artery Revascularization (TCAR)
Minimally invasive option to treat carotid artery disease.
Protection & Prevention
Treatment options for carotid artery disease depend upon the severity of the overall patient condition and symptoms. Moderate disease may not require an interventional procedure, as some individuals can manage the disease with medications and lifestyle changes. More severe blockages may require surgery. A potential complication of surgery is a stroke during the procedure itself. For patients at higher risk for the open surgical procedure, the TCAR Procedure is designed to reduce the risk of stroke while inserting a Stent.